As several countries in West Africa continue to struggle with the worst Ebola outbreak in history, the news worldwide has been flooded with stories about the mysterious and horrifying virus.
Photos of victims with the telltale hemorrhagic rash, bleeding from the eyes, ears, and nose, and stories of the stricken vomiting and coughing up blood add to the terror associated with this deadly virus.
But what exactly IS Ebola, and how does it kill?
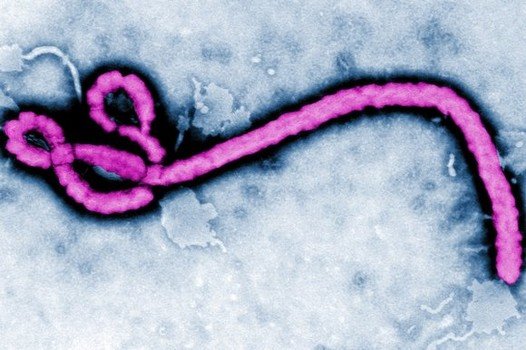
Ebola is an infection with a virus of the family Filoviridae, genus Ebolavirus. So far, only two members of this family of viruses have been identified – Marburgvirus and Ebolavirus. Five subspecies of Ebolavirus have been identified, four of which can cause disease in humans:
- Ebola virus (Zaire ebolavirus)
- Sudan virus (Sudan ebolavirus)
- Taï Forest virus (Taï Forest ebolavirus, formerly Côte d’Ivoire ebolavirus)
- Bundibugyo virus (Bundibugyo ebolavirus)
The fifth subspecies, Reston virus (Reston ebolavirus), is the one that has not caused disease in humans (but it can be fatal in non-human primates). This is the strain that killed dozens of lab monkeys at a research facility in Reston, VA, in 1989. Four workers at that facility tested positive for Ebola. In 1996, nine lab workers were exposed to this strain after handling infected animals. None of those infected developed symptoms or became ill, but they did develop antibodies to the strain. It is possible that the Reston strain can be transmitted via small-particle aerosols (airborne), but that hasn’t been confirmed.
Filovirus infections are transmitted via close personal contact with an infected individual or their bodily fluids (including through contact with contaminated medical equipment).
According to the CDC, “although in the laboratory the viruses display some capability of infection through small-particle aerosols, airborne spread among humans has not been clearly demonstrated.”
A study released last week showed that the strain causing the current outbreak in West Africa has gone through a surprisingly high amount of genetic drift. Those mutations may make treatment and diagnosis harder.
But can those mutations make Ebola virus change enough to become truly airborne, like the flu?
In his article Can Ebola Go Airborne? Dr. Scott Gottlieb said it is possible, but unlikely:
The widespread belief is that the Ebola virus would be very unlikely to change in a way that would allow the individual virus particles to be concentrated, and remain suspended in respiratory secretions — and then infect contacts through inhalation. The Ebola virus is comprised of ribonucleic acid (RNA). Such a structure makes it prone to undergoing rapid genetic changes.
But to become airborne, a lot of unlikely events would need to occur. Ebola’s RNA genome would have to mutate to the point where the coating that surrounds the virus particles (the protein capsid) is no longer susceptible to harsh drying effects of being suspended in air. To be spread through the air, it also generally helps if the virus is concentrated in the lungs of affected patients.
For humans, this is not the case. Ebola generally isn’t an infection of the lungs. The main organ that the virus targets is the liver. That is why patients stricken with Ebola develop very high amounts of the virus in the blood and in the feces, and not in their respiratory secretions.
Regarding the chances of an outbreak occurring in the United States, Dr. Gottlieb had this to say:
We will certainly see cases diagnosed here, and perhaps even experience some isolated clusters of disease. Health-care workers in advanced Western nations maintain infection controls that can curtail the spread of non-airborne diseases like Ebola.
The current outbreak in West Africa is caused by the Zaire ebolavirus. If infection is properly diagnosed quickly, and treatment is given promptly, a full recovery is likely.
However, the very nature of the Ebola virus can make early detection tricky. Early symptoms are similar to those of many far less harmless diseases. Fever, headache, weakness, diarrhea, and vomiting often present in the early stages, and can lead to a misdiagnosis – and delayed treatment.
What is intriguing – and terrifying – about Ebola is that the virus itself doesn’t kill people – the immune system’s reaction to it does.
“The normal job of the immune system is to eliminate infections,” virologist Christopher Basler explained to NPR. “But when it’s activated at extreme levels or it’s out of control, it becomes damaging to the host.”
In his article titled Ebola: A Dangerous Virus, But How Does it Really Kill?, Professor Edward Oparaoji explains how Ebola invades the body and causes the immune system to go into overdrive:
It disguises itself and stealthily evades detection and “arrest” by the “security guard” – dendritic cells and macrophages. Once inside and secured, the virus disarms the “security guard” rendering them incapable of sending signals for help to the protective “commandoes” – the antibodies and cytokines, to eliminate the “suspect” Ebola. As a result, the virus starts to multiply and invade more cells with reckless abandon, unchallenged, causing cells to die and explode. It is at this stage that the (host) immune system suddenly becomes aware that it has been overrun.
He goes on to explain how the immune system responds:
It then begins a belated over the top uncoordinated defense, launching its entire immunological arsenal at once, through massive release of cytokines – the (host) immune system equivalence of “shock and awe” response to the already widely spread virus. This most extreme immune response, which also signals the terminal phase of the infection, is referred to as the “cytokine storm”- It is this cytokine storm, the host response to the Ebola that kills. During this condition, the (host) immune system turns on itself, attacking every organ in the body, bursting blood vessels and making the infected person bleed both internally and externally, through the orifices (eyes, nose, etc.). This also involves vomits and diarrhea, causing severe low blood pressure and/or hypotensive shock and subsequently, death.
Other viral infections like Bird Flu and SARS can cause the immune system to launch an intense attack as well, but not with as much ferocity as it does with Ebola.
Survival requires stopping the cytokine storm and resulting hypotensive shock from occurring. Professor Oparaoji explains how this is done:
This can be accomplished through appropriate timely Anti-Ebola drug (ZMapp) or vaccine treatment, when available, and/or aggressive effective supportive treatment – such as maintenance of oxygenation, fluid and electrolyte therapy, blood pressure control with vasopressors, prevention and treatment of secondary infections, pain control and nutritional support, among others.
He also points out that treatment with the ZMAPP drug and Nigeria’s supportive treatment protocol don’t yield results that are that much different: 33% of people treated with ZMAPP have died, compared to 40% who were treated per Nigeria’s standard supportive treatment.
Medical missionaries Dr. Kent Brantly and Nancy Writebol were the first people to use ZMAPP. Both received supportive care at Emory University Hospital in Atlanta, and both have fully recovered. Dr. Brantly also received a unit of donated blood from a 14-year-old boy who recovered from Ebola. Similar treatment (via plasma antibodies) was used in an outbreak in 1995, with stunning results: 7 of the 8 treated with blood from convalesced patients survived.
But was their recovery due to the use of ZMAPP or something else?
At this point, we don’t know:
“They are the very first individuals to have ever receive this agent,” Dr. Bruce Ribner, director of Emory’s Infectious Disease Unit, told a news conference. “There is no prior experience with it, and frankly, we do not know whether it helped them, whether it made no difference, or even, theoretically, if it delayed their recovery.”
Doctors who have experience treating Ebola say that early and aggressive supportive care (like the care Professor Oparaoji described) is crucial to recovery. The physical condition of a person infected with Ebola also matters:
“And clearly for any acutely ill patient, nutritional status is extremely important,” Ribner said. “If you have somebody who’s well-nourished and somebody who is poorly nourished and they suffer the same illness, infectious or otherwise, the person with better nutrition has better survival outlook.”
ZMAPP is one of several Ebola treatments being developed. But, no matter which drug – if any – proves to be a useful treatment, time will be of the essence. It only takes viruses a few days to replicate and spread, and once the damage becomes widespread it can be impossible to reverse.
Regarding treatment with the blood of convalesced patients, well, it has been said that it would take a lot of plasma to make that a viable option. At this point, it doesn’t appear that anyone is seriously pursuing the use of that treatment modality, although there has been some discussion about it.
As with any disease, an ounce of prevention is worth a pound of cure.
For information on how to prepare for an Ebola outbreak in your area, please see Prepping for an Ebola Lockdown: No one goes out, no one comes in.

Vitamin D suppresses cytokine storm in the case of influenza, while also supporting targeted immune function. This much is well known. I’d like to know what the effect of vitamin D would be on Ebola outcome also. I’ve seen suggestions that Ebola outbreaks happen during the rainy and short dry seasons (as opposed to the long dry season in northern winter). Exactly when vitamin D levels will be at their lowest, particularly among dark skinned people.